Decoding “Cold” Tumors: Why Immune Evasion Remains a Challenge
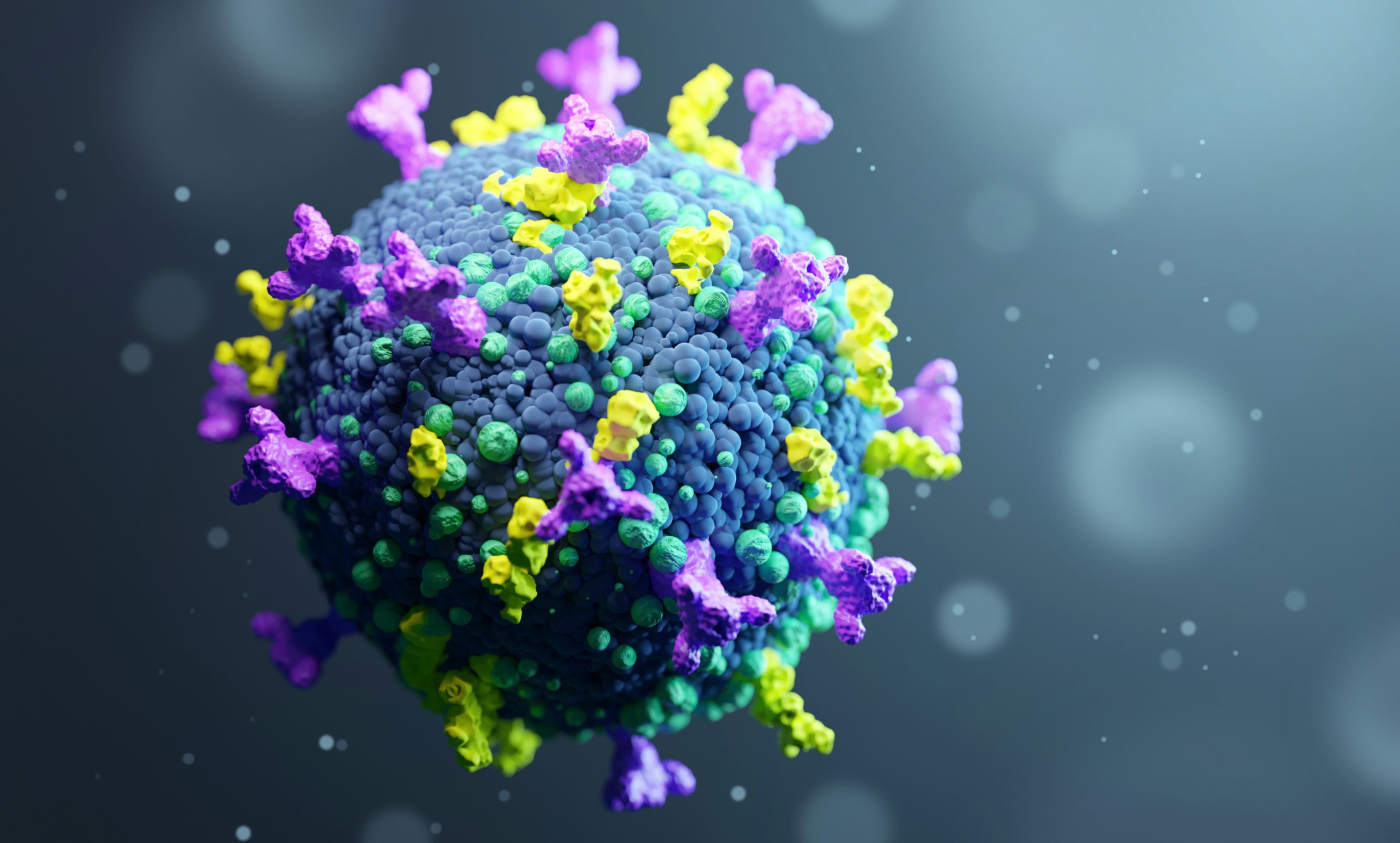
One of the most persistent obstacles in cancer immunotherapy is the challenge posed by “cold” tumors, which lack sufficient immune cell infiltration. These tumors fail to provoke a strong immune response, making them less responsive to treatments such as checkpoint inhibitors or CAR-T cell therapy. The scarcity of neoantigens and absence of inflammation within the tumor microenvironment often hinder recognition by the body’s immune defenses, allowing malignant cells to proliferate undetected. This invisibility to the immune system significantly reduces the efficacy of immunotherapies designed to harness the body’s natural defenses against cancer.
Traditional approaches to targeting “cold” tumors have focused on increasing antigen presentation or altering the tumor microenvironment through radiation, chemotherapy, or combination therapies. However, these interventions often require extensive trial-and-error experimentation. Artificial intelligence, particularly large-scale models like Google’s C2S-Scale 27B, offers a strategic advantage by identifying molecular pathways that are not immediately apparent through conventional laboratory methods. By accelerating hypothesis generation and testing, AI systems are reshaping how researchers approach the biological complexity of immune-evasive cancers.
Google’s C2S-Scale 27B Model: A New Tool for Biomedical Discovery
The Cell2Sentence-Scale 27B (C2S-Scale) model developed by Google is a transformer-based AI system trained to uncover relationships across cellular biology, molecular interactions, and therapeutic outcomes. With 27 billion parameters, it has the capacity to analyze structured and unstructured biomedical data, including genomic sequences, molecular pathways, and scientific literature, to generate predictions that can be tested in experimental settings. This model was instrumental in identifying a potential combination therapy for cold tumors involving silmitasertib, a casein kinase 2 inhibitor, and interferon-alpha.
In collaboration with Yale University, researchers used the model’s predictions to hypothesize that combining silmitasertib with low-dose interferon could significantly increase the presentation of tumor-associated antigens. Yale’s validation in human neuroendocrine cell models confirmed the synergistic interaction of the two agents, achieving nearly a 50% increase in antigen presentation compared to individual treatments alone. This result was particularly important because it offered a tangible method to convert cold tumors into “hot” tumors, which are more amenable to immune system targeting and immunotherapy-based interventions1.
From Prediction to Practice: The Role of AI in Accelerating Validation
One of the major bottlenecks in translational medicine is the time required to move from theoretical discovery to experimental validation. AI models like C2S-Scale 27B dramatically
Read-Only
$3.99/month
- ✓ Unlimited article access
- ✓ Profile setup & commenting
- ✓ Newsletter
Essential
$6.99/month
- ✓ All Read-Only features
- ✓ Connect with subscribers
- ✓ Private messaging
- ✓ Access to CityGov AI
- ✓ 5 submissions, 2 publications
Premium
$9.99/month
- ✓ All Essential features
- 3 publications
- ✓ Library function access
- ✓ Spotlight feature
- ✓ Expert verification
- ✓ Early access to new features
More from Artificial Intelligence
Explore related articles on similar topics